By Simon Albaugh – YAN – Garden City.
COVID-19 has brought the question of safety to the forefront of everyone’s mind. Whether it be the constant hand-washing that we’ve all needed to do, or the masks that have suddenly appeared in the places we go, this crisis has called our all of health into question. But there are people whose health has always been in crisis, and the Novel Coronavirus Pandemic has made caring for vulnerable people even harder.
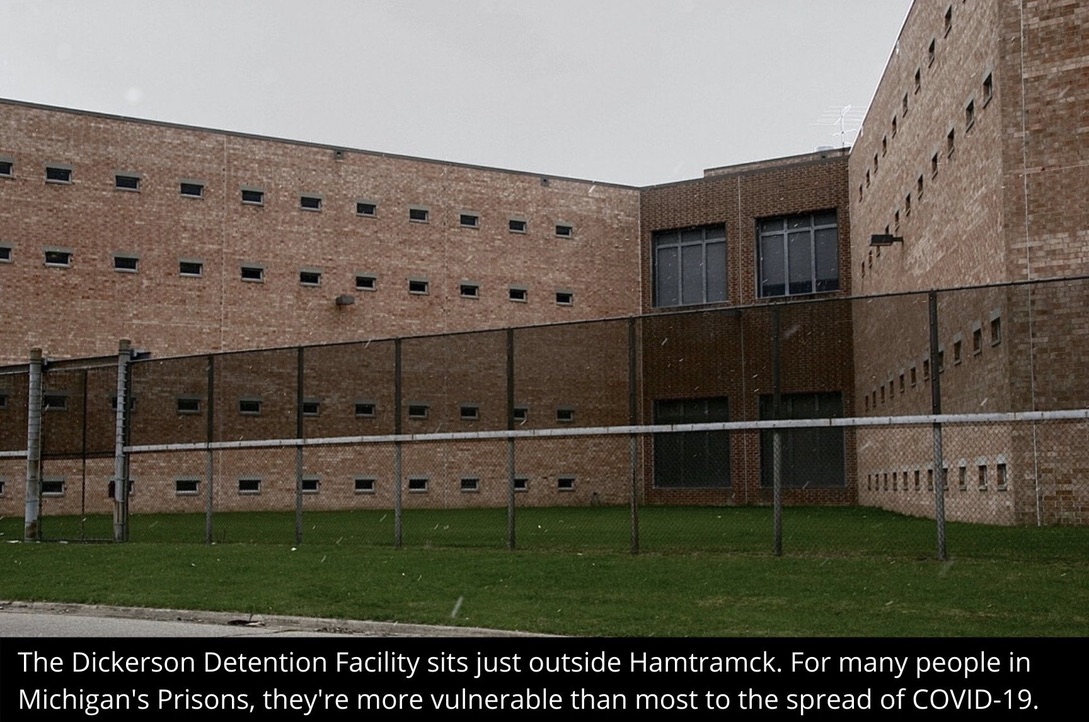
In the area’s homeless shelters, psychiatric facilities, jails and prisons, the populations they house are at a much higher risk of contracting the COVID-19 illness. The communal living situations that are especially common in these institutions have made a logistical nightmare for those who work every day to keep these people safe.
Takwah Saleh works as a recreational therapist at a Psychiatric Hospital in Garden City. Before the pandemic, she was responsible for all the activities that would help the patients stay active and healthy. Now, she’s responsible for other activities.
“We made folders for the patients for word searches, books, magazines, newspapers,” Saleh said. “Things for them to do in their room.”
Since the COVID-19 Crisis in Michigan started at the beginning of March, institutions like the Hospital where she works have needed to act fast in slowing the spread of the Novel Coronavirus among residents. Major changes like visitor restrictions and leave restrictions have affected the patients’ wellbeing.
The workers of the hospital – the doctors, nurses, therapists and supporting staff – have all had to make changes to keep up with precautions too. Protective gear is a must when caring for patients in a communal living environment.
“We get our temperature taken right at the door,” Saleh said. “We have no outside visitors. And we get a new mask every day.”
Patients in each of the Hospital’s five units have been forced to stay in their rooms for most of their time, in order to maintain some level of social distancing. The little exercise that they’re able to do happens in the hallways of the units now. All this has played a difficult role in exacerbating the patients’ illnesses.
Saleh says that many of the patients don’t quite understand what’s happening. In the unfortunate circumstances when someone does develop symptoms of COVID-19, their trip to another hospital can be traumatizing.
The ones who do understand, typically the higher-functioning younger population, have been taking the crisis very seriously. They wash their hands, keep their distance and understand that they don’t want to get sick too.
But there are patients who aren’t quite able to understand. The lower-functioning patients have a difficult time cleaning their hands and keeping their distance from one another.
“We have a big number of patients who don’t get it and don’t understand,” Saleh said. “They’re in your face, like really close. Or they’ll get close to other patients. If one gets sick, it’s hard for them.
For right now, Saleh says that the hospital has to work around a large group of people who have been confirmed to carry the COVID-19 Illness. Like many other places with difficult living circumstances, the job carries its risks for infection.
Chrissy Sowri works as a corrections officer. Her job involves working very intimately with the state’s Prison Population – another especially vulnerable group who are more likely to contract the COVID-19 illness.
Like the people who are living in the Walter Reuther Psychiatric Units, the prison population is generally taking this issue very seriously. However the precautions the corrections officers are taking is slightly different.
Sowri says that everyone has their temperature taken before they go to their work detail or to the day room. The day room also has limited the number of people who can spend time there, meaning that inmates spend more of their time inside their cells.
“They’ve been compliant with the new rules,” Sowri said. “Most are afraid of getting sick, so they have no problem with it really. And they have even started to police themselves in a way on wearing the mask.”
Tensions about spending more time in their cells, restrictions on visitors and other measures have also risen during the crisis. Sowri says that inmates aren’t necessarily more violent, but definitely are more antsy during this time.
Most of the inmates at the jail are given reliable information about the developments outside. They’re given reliable news while they spend their time. When new recommendations come, the inmates are often in the know as the recommendations are updated.
Vulnerable populations like psychiatric hospital patients and prisoners have a unique challenge during this time. They’re much more likely to contract the COVID-19 illness when any one of them is infected. And the workers who care for these populations are in a difficult place, keeping up with new protocol while they try to stay safe themselves.